)
Fasting and Cancer Prevention and Management
Fasting and Oncology: Here is what a Nutritionist thinks
Humans have been fasting since the beginning of time, whether due to food scarcity, religious reasons, or for weight loss or vanity purposes.
Historically, as hunter gatherers, alternating periods of feast and famine was simply the way of life. With industrialisation and increased grain farming and processing came a reliance on highly processed convenience foods to feed an ever growing and busy population. These days we even have 24hour supermarkets and delivery services providing access to food and drinks at all hours of the day and night, resulting in constant feast and very little famine. Not surprising that obesity and related chronic diseases are the highest they have ever been.
Whilst epidemiological and observational studies look particularly into the impacts of religious fasting patterns, controlled short term or periodic fasting is getting renewed interest in clinical research both a weight management perspective, but also to investigate potential benefits in the prevention of chronic disease. Through structured clinical trials, researchers are finding improvements in various health parameters and blood markers in those who do some form of regular fasting. These parameters include lower blood glucose levels, lower insulin levels, improvement in HbA1c (insulin sensitivity), improvements in hunger and satiety signalling, as well cholesterol and inflammation markers. It has been found that regular and controlled restriction of caloric intake results in improvements in physiological functioning and metabolism, enhances performance, slows cellular ageing, and helps prevent chronic disease processes including cardiovascular disease, type 2 diabetes, neurodegenerative conditions, cancer and more.
Fasting is done by restricting or avoiding any calorie containing foods or drinks for a meaningful period of time. There are many models of fasting available, including but not restricted to:
- Alternate day fasting: cycling between one day of no energy containing foods or drinks consumed, followed by one day of unrestricted consumption.
- Time restricted feeding, also known as Intermittent Fasting or Extended Overnight Fasting: involving a longer period each night without calorie consumption, followed by a narrow window (eg 8-10 hours) of unrestricted consumption during the day
- The 5:2 approach: 2, non-consecutive days per week of severely restricted eating (maximum 500 calories), with unrestricted food consumption on the other 5 days per week
- Fasting mimicking diets: severely calorie restricted feeding (eg 500 calories only) for a period of consecutive days, usually 3-7, which may be repeated periodically throughout the year.
Levels of evidence for the above approaches do vary, and there is certainly variability in what suits different people and situations. For example, Intermittent and Alternate Day fasting cause more frequent but less pronounced changes than some of the other, more prolonged approaches. Fast for too long, and there may be detrimental effects such as muscle wastage, compromised immune function and more. The optimal length and frequency of fasting periods is yet to be determined and may in fact vary from person to person. Lifestyle factors and exercise levels may further impact the benefits of fasting, suggesting that targeted fasting regimens should be part of a holistic and multi-pronged approach to wellness and preventative care.
But is fasting useful for the management of cancer, and what are its effects in conjunction with current treatment protocols?
Integrative Oncology explained by a Nutritionist
Integrative Oncology aims to safely combine (ie integrate) approved and standardised conventional medical approaches with evidence based complementary therapies to improve the patient’s experience and treatment outcomes.
One of the biggest challenges in Integrative Oncology is the risk of a potential interaction between a complementary intervention, such as a nutritional supplement, and a drug or other medical treatment approach. For example, it is known that some nutritional or herbal medicines may compete with pharmaceutical drugs for absorption in the gut, others may slow or accelerate detoxification processes in the liver, changing serum levels of the active drug in the system and thereby affecting treatment efficacy. Integrative Oncology Specialists spend countless hours on evolving research to understand what exactly these pharmacokinetic or pharmacodynamic interactions are and how to safely recommend complementary therapies without negatively impacting the patient’s medical treatment efficacy. It goes without saying that it is highly discouraged for patients to self-prescribe over the counter natural supplements while in treatment.
Fasting is far less likely to impact the pharmacodynamic or pharmacokinetic variability of medical treatments. (Do note, some medications are recommended to be had WITH or WITHOUT food as this may affect absorption or prevent side effects such as nausea – always follow the recommendations of your medical practitioner or on the medication instruction leaflet).
Controlled and supervised fasting has largely been found to be safe in the clinical setting (with some exceptions). It is inexpensive and, as research suggests, can be beneficial for chronic disease management and overall health parameters, as mentioned above. There are many clinical trials currently underway investigating the impacts of various fasting models and their safe use in Integrative Oncology care.
Fasting explained by a Nutritionist
Metabolic regulation of the body is highly dependent on levels of blood sugar and insulin, blood lipids (eg cholesterol), hormones, neurotransmitters and inflammation regulators. It is long known that chronic imbalances of these are highly linked with increased risks of metabolic disturbance or metabolic syndrome, cardiovascular disease, type 2 diabetes, neurodegenerative conditions as well as cancer.
Fasting is achieved by a period of abstinence from calorie containing foods or beverages. Once a food or drink is consumed, digestive processes commence to absorb nutrients into the blood stream, which in turn cause many chain reactions that affect the physiology of the body. Especially carbohydrates have a significant impact – carbohydrates are digested into glucose (simple sugars), and the elevation of blood sugar levels activate insulin release, cortisol production, cellular growth, and lipogenesis (fat production and storage) amongst others. If the body isn’t fed for a number of hours, blood sugar and insulin levels drop, signalling to the body to activate other physiological processes including cellular adaptation and stress resistance. The parasympathetic nervous system is activated to support digestion, lower blood pressure, downregulate growth factor signalling, inflammation and oxidative stress, and activate of autophagy (the degradation of damaged cells).
The body’s biochemistry is carefully regulated to survive those fluctuating conditions. Intermittent fasting protocols aim to mimic historical eating patterns, and essentially negate the disruption in physiology by modern cultural and social overeating patterns.
Fasting and Cancer
Decades ago, a string of animal studies showed that chronic caloric restriction (without malnutrition) is one of the most effective interventions for cancer prevention. It results in reduced tumour growth via the downregulation of insulin-driven growth factors, inflammatory cytokines, and anabolic hormones as well as decreased oxidative stress and free-radical–induced DNA damage. Applicability or chronic caloric restriction in humans though is limited due to challenges with long term sustainability, as it quickly results in malnutrition. Thus, intermittent and periodic fasting approaches are being examined as more practical and sustainable alternatives.
Contemporary research shows that targeted intermittent or periodic fasting may equally support the prevention and the treatment of cancers. Animal studies found that short fasting interventions (usually 24 – 48 hours in length) can slow tumour onset and growth in various tumour streams. Other studies looking at alternate day fasting for 2 weeks also found improved survival compared to the control group, without significant weight loss.
Physiologically, a number of things happen:
First and foremost, there is the reduction of blood sugar levels, insulin and IGF-1 (an insulin-like growth factor implicated in many cancers). This in turn signals a reduction of c-peptide and leptin, relevant in some cancers, and an increase in adiponectin, which inhibits cancer cell growth and metastasis via the activation of the AMPK pathway. Various other biochemical pathways are modified in a fasting state: cell cycle regulation and timely cell death is activated, encouraging replenishment of new, healthy tissues. It also reduces production of various growth-promoting inflammatory markers such as interleukins, CRP and TNF-alpha, and upregulates genes that promote cell repair and autophagy.
Further physiological processes positively impacted by fasting regimens include circadian biology and the gut microbiome, again both relevant to cancer prevention and management. When we sleep, the body rests and repairs, driven by the body’s master antioxidant melatonin, which regulates important repair processes that bolster cellular protection and autophagy. The microbiome is altered in those groups that fast regularly and that have sound sleep-and-wake cycles, suggesting an interrelationship between the three. Studies show that microbiome health and diversity is incredibly important for immune function, management of inflammation, not to mention nutrient digestion and absorption, and the prevention of chronic illness and many types of cancer.
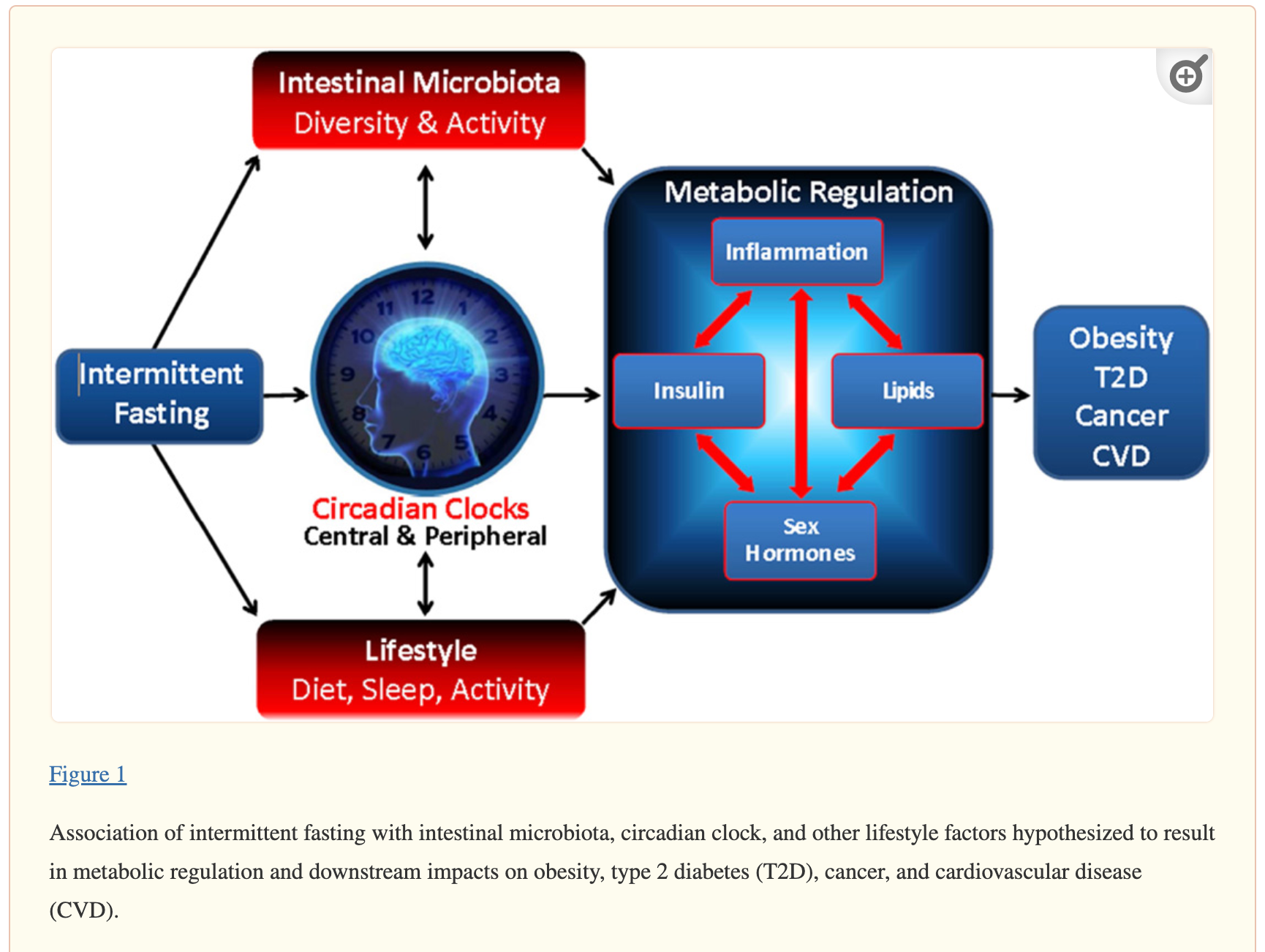
Source: Patterson et al (2015) Intermittent Fasting and Human Metabolic Health
Now, while preclinical evidence for the above is promising, unfortunately human clinical trials are still lacking, and one can only draw so many conclusions between a mouse and a human. When it comes to a person with an active cancer, many more factors need to be taken into consideration, including current nutritional and metabolic health, organ and digestive function, tumour load, stress levels and much more. For should the fasting period pass the optimum length of time, additional signals are activated that indicate starvation, ie chronic nutritional insufficiency. This is considered a detrimental stress factor that results in healthy cell degeneration, muscle wastage and cachexia, which in turn results in weakness, reduced ability of the body to tolerate treatment, a reduced ability to fight infection, and is associated with poorer cancer prognoses.
Furthermore, some studies suggest that fasting may also result in “rebound growth” during the refeeding period after a fast, something that patients with cancer naturally want to avoid. The real sweet spot seems to be when there is regular metabolic switching between fasting and feeding periods. This allows optimisation of physiological wellness processes whilst also giving cells needed time to recover from the stress of a fasting period. The only problem is, we do not know when this is, and there may be variability from person to person. Hmmmm...
Fasting around chemotherapy
Once again, preclinical evidence (ie models and animal studies) into the use of fasting around chemotherapy and radiotherapy is promising. Studies are showing that fasting has the potential to protect normal cells from the toxicities of treatment, while sensitising cancer cells to its damaging effects, therefor decreasing cancer cell growth and enhancing treatment efficacy. This phenomenon is known as “differential stress resistance”: healthy cells can activate protective mechanisms during short periods of stress, while cancer cells, due to their upregulated oncogenes, are unable to, rendering them more vulnerable to the effects of treatment.
In layman’s terms, this results in less damage to healthy cells, and more damage to cancer cells – exactly what we want, woohoo!
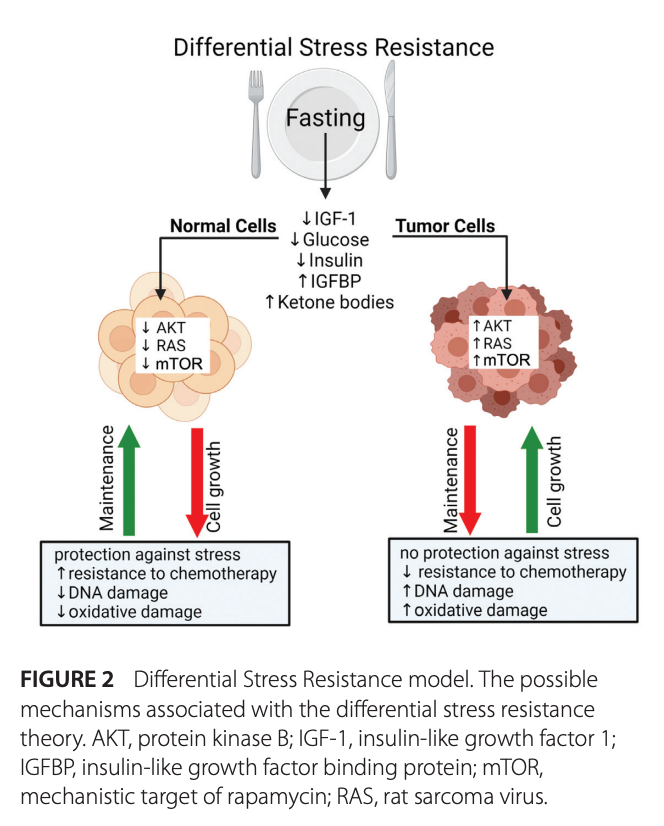
Source: Gabel et al (2021) Current evidence and directions for intermittent fasting during cancer chemotherapy
But unfortunately, human trials are still scarce (seeing a repeat pattern here?). There are a few that look at the effect of fasting on chemotherapy side effects, however they are mostly anecdotal. Nevertheless, patients report reduced levels of nausea, gastrointestinal distress, mucositis, and less pronounced fatigue if they conducted a short term fast around their chemotherapy treatment.
Regarding treatment efficacy, two small human trials into short-term fasting, and one trial looking at a fasting mimicking diet around chemotherapy, do suggest positive effects, including improved treatment response. However, these studies are also underpowered due to small sample sizes, heterogeneity of the patient groups, or lack of control groups.
The unanimous conclusion is that there may be vast opportunity here for the use of controlled fasting methods to reduce treatment side effects and support patient outcomes. Luckily, many trials are currently underway to exactly assess impact on tumour growth rates and treatment efficacy, underlying mechanisms and of course safety and tolerability. This is an exciting space to watch.
So would we recommend fasting alone as a treatment? No.
Aside from the very real risks mentioned above, research suggests that chemotherapy and fasting work best in controlled synergism: the idea that cancer can be treated just by fasting for weeks on end, as was made popular decades ago, has been debunked: fasting alone is not sufficient to cause any improvement in cancer-free survival, and time and time again the negative effects cause a real compromise to a person’s health and much poorer overall outcomes.
Conclusion
Short-term, controlled and flexible fasting regimens are currently being researched as inexpensive yet potentially powerful adjuncts to standard cancer treatment protocols. Preclinical models suggest targeted fasting around chemotherapy or radiation may reduce treatment side effects and enhance treatment efficacy, and human trials to assess safety, tolerability and underlying mechanism are underway. There seems to be a fine line between short term, beneficial nutrient deprivation and unhealthy malnutrition or starvation, which has the ability to backfire on a patient’s health and wellness. As we await further research outcomes regarding the ideal methods and timing of fasting, practitioners are urged to proceed with caution, and if deemed appropriate to personalise fasting protocols, applying them in a sensible, flexible and short term manner, tailored to the health and needs of each individual. This means, if you are going to fast in any meaningful way, it must be under the guidance of an experienced clinical nutritionist.
NOTE: Fasting periods lasting longer than 24 hours and particularly those lasting 3 or more days should be done under the careful supervision of a Nutritionist and Medical Doctor. Fasting is not safe in children, pregnant women or the elderly. Always consult a practitioner before making any changes to diet and lifestyle.


)
)










Tags: